Pixabay
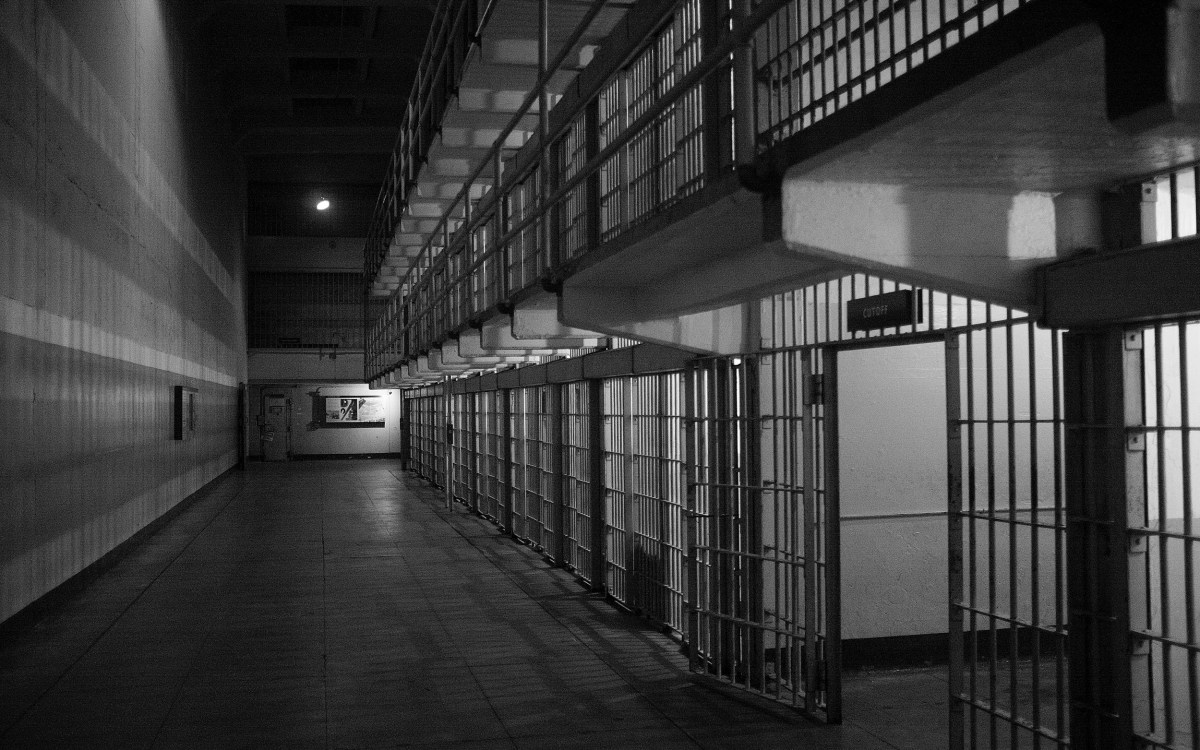
Assessing the effect of the COVID-19 pandemic on correctional institutions
Working in real time, Harvard researchers are surveying correctional facilities to find out how they are being affected by the pandemic
This is part of our Coronavirus Update series in which Harvard specialists in epidemiology, infectious disease, economics, politics, and other disciplines offer insights into what the latest developments in the COVID-19 outbreak may bring.
Across the country and the world, communities are working feverishly to measure the coronavirus pandemic’s impact — struggling with shortages of tests and depleted health care capabilities to gauge the numbers of the infected, the sick, and the dead.
Accurate data is the first vital step in understanding the scope of the problem and developing and calibrating the best response. But, as the world moves to lockdown and social isolation, what is happening to the approximately 2.3 million people behind bars in the United States and to the tens of thousands who work in those facilities — line officers, administrators, nurses, therapists, doctors?
Harvard Kennedy School Professor of Public Policy Marcella Alsan and Harvard Law School Professor of Law Crystal Yang have teamed up with the National Commission on Correctional Health Care (NCCHC) to conduct the first detailed survey on the coronavirus pandemic’s impact on the country’s prisons, jails, and juvenile detention facilities. HKS discusses their groundbreaking work, what it tells us about the spread and treatment of the disease among some of the most vulnerable populations, and how this valuable data can guide practitioners and policymakers.
Q&A
Crystal Yang and Marcella Aslan
Harvard Kennedy School: How did you both come to find yourself working with the NCCHC as the pandemic struck?
Crystal Yang: Marcella and I are both economists who are interested in using policy to improve outcomes for vulnerable and underrepresented populations. We have been collaborators for some time on issues at the intersection of the criminal justice system and the health care system. We each bring a complementary skill set to the table, with Marcella’s dual training in medicine and economics and my dual training in law and economics. Prior to the start of the pandemic, we had partnered with the NCCHC to better understand the unique health care needs of incarcerated populations and the role that health care standards and accreditation can play.
Once the pandemic struck, we were gravely concerned about the impact that COVID-19 would have on inmates, correctional officers, and health care staff. But we quickly realized that nationwide, real-time data did not exist. To address this data deficit, we quickly worked together with our partners at NCCHC (including CEO Deborah Ross and Brent Gibson, their chief health officer) to develop high-frequency surveys in order to assess the needs and preparedness of correctional facilities across the United States in dealing with the pandemic.
Gibson notes: “This partnership has been extraordinary, and I don’t use that word lightly. The Harvard team is as responsive and knowledgeable as any I have worked with in my nearly 20-year medical and public health career. The tools and expertise they bring have made this whole effort possible.”
“As the pandemic continues to spread, policymakers should implement criminal justice policies that can protect the health of inmates and correctional staff without endangering public safety.”
Crystal Yang
HKS: What are you finding?
Marcella Alsan: So far, we have collected data from more than 320 facilities housing approximately 10 percent of the country’s inmates across 47 states. While not necessarily representative of all correctional institutions, the results nonetheless are vital for policymakers responding to the pandemic in their own states and communities. NCCHC has assured me that even this level of response is extremely encouraging, as correctional programs are not always willing to share information.
In terms of specifics, we found that, between the initial survey on March 25 and the latest follow-up on April 3, the number of reported COVID-19 cases among participating correctional facilities increased rapidly. The highest number of reported cases was among correctional staff — including health care staff and correctional officers. Specifically, the number of COVID-19 cases among staff increased from 136 to 245 among approximately 100 facilities that consistently reported on a daily basis. During the same period, the number of cases among inmates increased from 32 to 67 among approximately 100 facilities that consistently reported. In addition, there were two reported deaths among correctional staff.
Combining the survey data with COVID-19 case data from The New York Times, we found that states that have been especially hard hit by the pandemic, such as Michigan and New Jersey, are also locations where correctional officers are more affected. At the state level, reported correctional staff cases are also correlated with reported cases among inmates. In addition, about two-thirds of facilities stated they had adequate personal protective equipment (PPE) and 60 percent said they had access to lab testing. Correctional administrators and frontline staff underscored that these levels, though slowly growing over time, are still insufficient to protect both staff and inmates from disease spread.
HKS: What are the key takeaways for health care delivery in correctional facilities?
Alsan: What’s striking to me about these findings so far is that correctional staff are also at high risk, either because of community exposure or exposure in the facilities themselves. Therefore, keeping visitors out is unlikely to be a failsafe method to prevent infectious spread. Staff also need to have access to protective equipment and testing. In addition, many of the facilities surveyed recounted they were screening inmates using the only method they had readily available: temperature and symptom screening. Since COVID-19 can be transmitted asymptomatically, it would be much safer to empower all facilities to screen people using rapid lab tests. We also have anecdotal evidence that it may prove challenging for staff to practice social distancing in a correctional institution. NCCHC has assembled some practical guidance that will be helpful in addressing this.
HKS: What are the key takeaways for the criminal justice system?
Yang: Our findings suggest that as the pandemic continues to spread, policymakers should implement criminal justice policies that can protect the health of inmates and correctional staff without endangering public safety. Qualitative comments from participating facilities in our survey indicate a range of sound responses to the pandemic, including releasing medically vulnerable inmates, limiting pretrial detention for individuals charged with nonviolent or misdemeanor offenses, quashing nonviolent minor arrest warrants, and increasing the use of summons in lieu of arrests for nonviolent offenses.
Alsan and Yang are faculty affiliates of the Kennedy School’s Malcolm Wiener Center for Social Policy. They are both economists. Alsan also has degrees in medicine and public health, and has held hospital fellowships in global health equity and infectious disease. Yang served as a federal prosecutor and is also a faculty research fellow at the National Bureau of Economic Research.