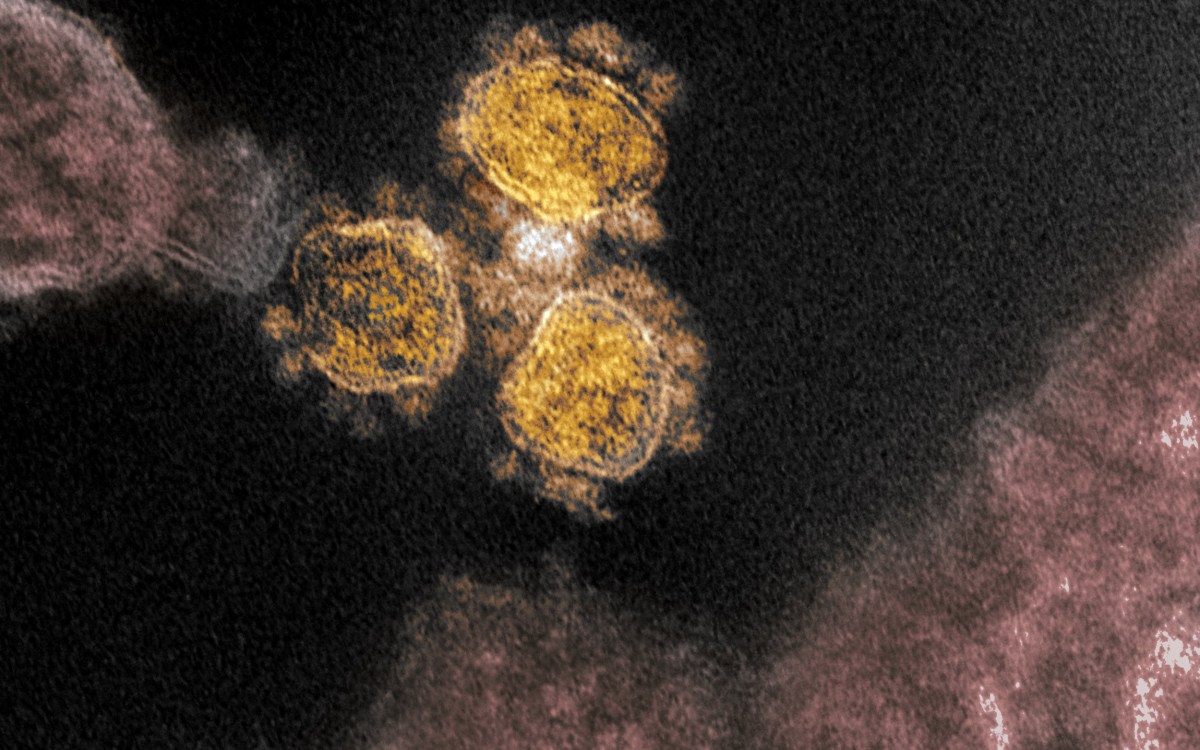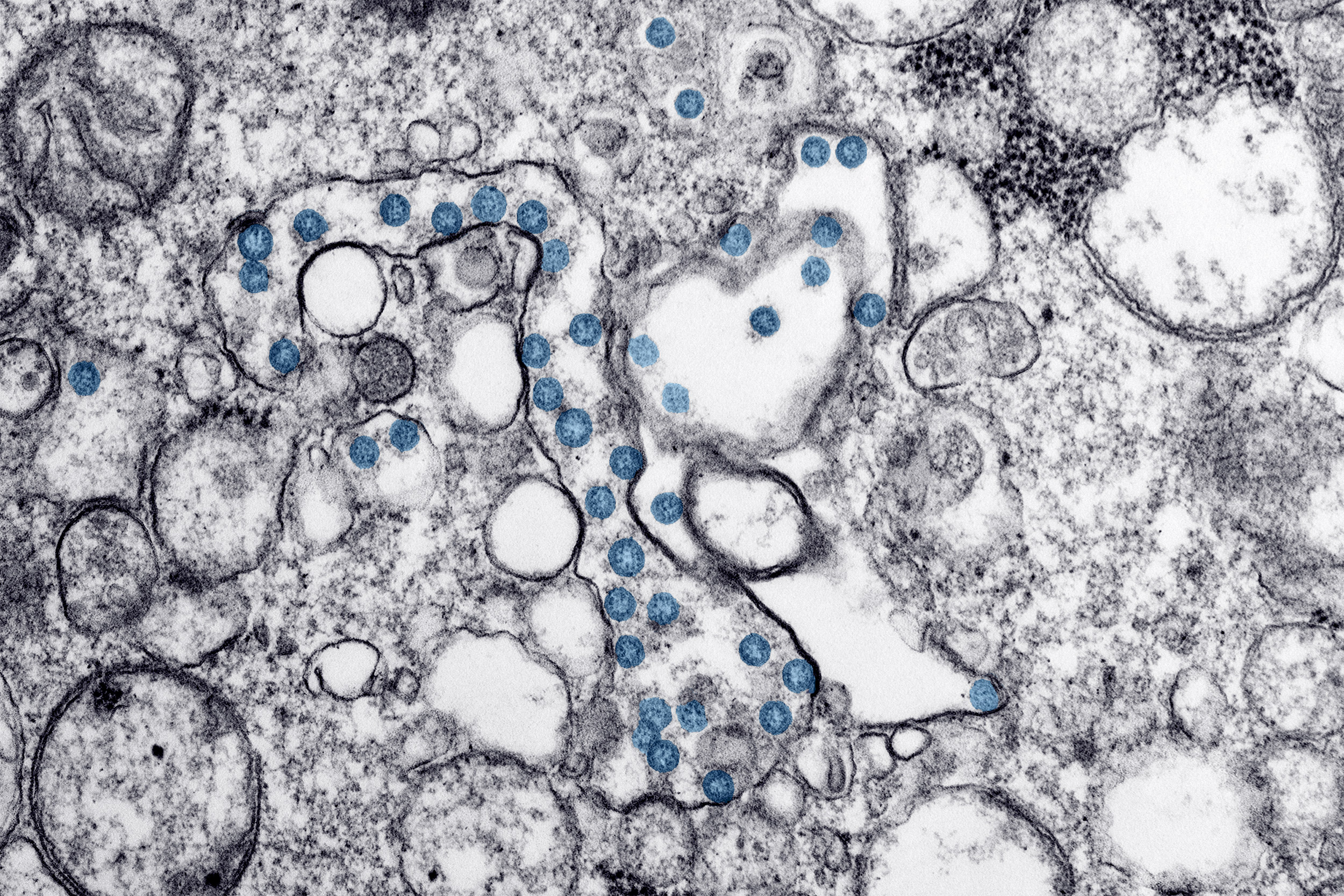
This is an image of an isolate from the first U.S. case of COVID-19, formerly known as 2019-nCoV.
Credit: CDC
Antibody evolution may predict COVID-19 outcomes
New study shows differences between patients who survived severe COVID-19 and patients who died from it
More like this
For COVID-19, the difference between surviving and not surviving severe disease may be due to the quality, not the quantity, of the patients’ antibody development and response, suggests a new Cell paper published by Galit Alter, a member of the Ragon Institute of MGH, MIT and Harvard.
The study, published in the journal Cell, used Alter’s systems serology approach to profile the antibody immune responses of 193 hospitalized COVID-19 patients, comparing responses from patients with moderate and severe disease and patients who passed away from COVID-19.
While all patients developed antibodies against SARS-CoV-2, the way the antibodies developed, or evolved, differed between the three groups. For patients that didn’t survive the disease, the antibody response never fully evolved.
“There was a significant defect in the development of IgG antibodies, which may be essential in the early control and elimination of the virus, ” Alter says. “Here, we were able to see the global impact of this defective IgG evolution, resulting in a compromised ability to promote essential viral clearing immune functions.”
In a mature immune response, antibodies both block infection and direct the immune system to kill infected cells. To guide the killer immune response, antibodies attach to the Fc-receptor, a “docking site” specific to antibodies that is found on all immune cells. Without strong Fc-receptor binding, antibodies may fail to grab and destroy virus following infection.
Compared to survivors, patients who passed from COVID-19 had antibodies that never fully developed the ability to strongly bind to Fc-receptors and therefore may not have been able to fully trigger immune killing activity.
Alter’s group, led by Tomer Zohar, Carolin Loos, Stephanie Fischinger, and Caroline Atyeo, also found that survivors’ immune systems could recognize and target an area of the SARS-CoV-2 spike protein known as the S2 domain. The S2 domain is found in other coronaviruses that infect humans, so patients whose antibodies can target it may have pre-existing immunity to the S2 domain because of exposure to other, common coronaviruses.
Patients with antibodies that can recognize S2 domains on different coronaviruses may be able to use this pre-existing immunity to generate killer antibodies faster and sooner following SARS-CoV-2 infection.
“If we can further understand the importance of cross-coronavirus immunity,” says Zohar, “researchers may be able to design vaccines able to counteract a much broader range of coronaviruses.”
With studies like these, Alter and her team are working to understand the nature of protective immunity against SARS-CoV-2, including partnering with COVID-19 vaccine developers, to help bring an end to this pandemic.