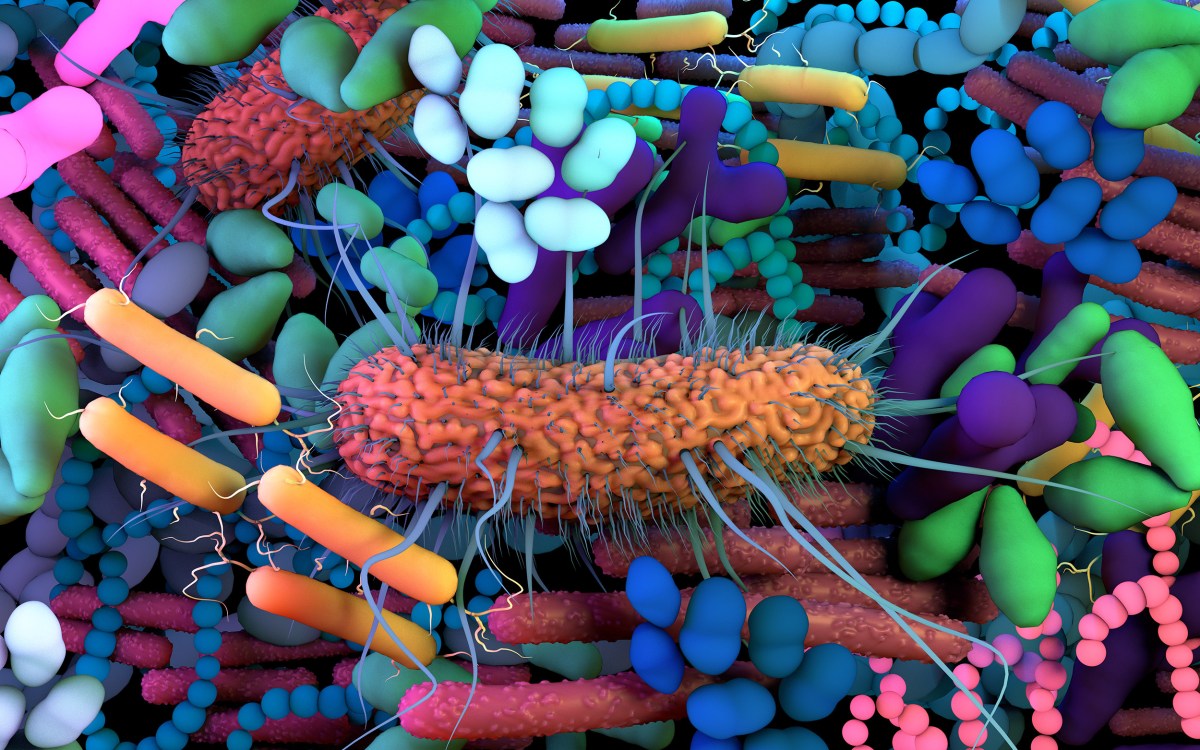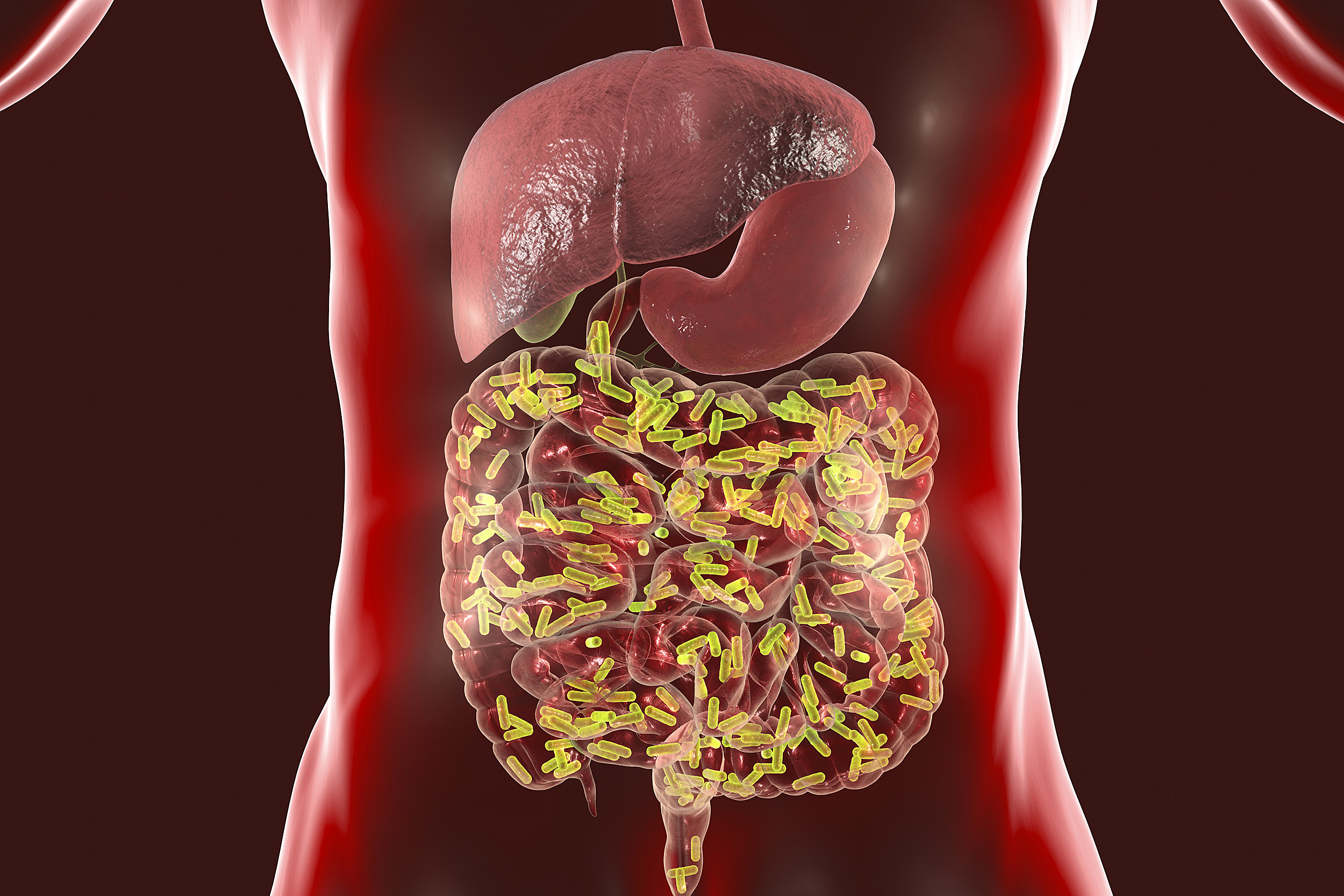
A 3D illustration of the intestinal microbiome.
iStock
A gut feeling
Scientists link genetic makeup of bacteria in the human gut to several human diseases
We are truly never alone, not even within our own bodies. Human beings play host to trillions of bacteria, fungi, viruses, and other microorganisms that make up the human microbiome. In recent years, the mix of these resident bacteria, and the presence of specific bacterial species, has been linked to conditions ranging from obesity to multiple sclerosis.
Now, going a step farther, researchers at Harvard Medical School and Joslin Diabetes Center have gone beyond microbial species. Analyzing the genetic makeup of bacteria in the human gut, the team has successfully linked groups of bacterial genes, or “genetic signatures,” to multiple diseases.
The work brings scientists closer to developing tests that could predict disease risk or identify disease presence based on a sampling of the genetic makeup of a person’s microbiome.
The findings, to be published May 18 in Nature Communications, link sets of bacterial genes to the presence of coronary artery disease, cirrhosis of the liver, inflammatory bowel disease, colon cancer, and type 2 diabetes. The analysis indicates that three of these conditions — coronary artery disease, inflammatory bowel disease, and liver cirrhosis — share many of the same bacterial genes. In other words, people whose guts harbor these bacterial genes seem more likely to have one or more of these three conditions.
The work represents a significant advance in the current understanding of the relationship between microbes residing in the human gut and specific diseases, the team said. If confirmed through further research, the results could inform the design of tools that could gauge a person’s risk for a range of conditions based on analysis of a single fecal sample, they added.
“This opens a window for the development of tests using cross-disease, gene-based indicators of patient health,” said first author Braden Tierney, a graduate student in the biological and biomedical sciences program at HMS. “We’ve identified genetic markers that we think could eventually lead to tests, or just one test, to identify associations with a number of medical conditions.”
The researchers caution that their study was not designed to elucidate exactly how and why these microbial genes may be linked to different diseases. Thus far, they said, it remains unclear whether these bacteria are involved in disease development or are mere bystanders in this process.
The goal of the study was to determine whether groups of genes could reliably indicate the presence of different diseases. These newly identified microbial genetic signatures, however, could be studied further to determine what role, if any, the organisms play in disease development.
“Our study underscores the value of data science to tease out complex interplay between microbes and humans,” said study senior author Chirag Patel, associate professor of biomedical informatics in the Blavatnik Institute at HMS.
The researchers started out by collecting microbiome data from 13 groups of patients totaling more than 2,500 samples. Next, they analyzed the data to pinpoint linkages between seven diseases and millions of microbial species, microbial metabolic pathways, and microbial genes. By trying out a variety of modeling approaches — computing a total of 67 million different statistical models — they were able to observe what microbiome features consistently emerged as the strongest disease-associated candidates.
Of all the various microbial characteristics — species, pathways, and genes — microbial genes had the greatest predictive power. In other words, the researchers said, groups of bacterial genes, or genetic signatures, rather than merely the presence of certain bacterial families, were linked most closely to the presence of a given condition.
“This opens a window for the development of tests using cross-disease, gene-based indicators of patient health.”
Braden Tierney
Some of the main observations included:
- Clusters of bacterial genes, or genetic signatures, rather than individual bacterial genes, appear implicated in various types of human disease.
- Coronary artery disease, inflammatory bowel disease, and liver cirrhosis have similar gut microbiome genetic signatures.
- Type 2 diabetes, by contrast, has a microbiome signature unlike any other phenotype tested.
- The analysis did not find a consistent link between the presence of the bacterial species Solobacterium moorei and colon cancer — an association previously reported in numerous studies. However, the researchers did identify particular genes from a S. moorei subspecies associated with colorectal cancer. This finding indicates that gene-level analysis can yield biomarkers of disease with greater precision and more specificity compared with current approaches. Patel said this result underscores the notion that it is not merely the presence of a given bacterial family that may portend risk, but rather the strains and gene signatures of the microbes that matter. The ability to identify interconnections with such precision will be critical for designing tests that can measure risk reliably, he added. Thus, in this specific example, a test intended to measure colon-cancer risk by merely detecting the presence of S. moorei in the gut may not be as reliable as a more refined test that measures bacterial genes to detect the presence of specific strains of S. moorei that are associated with colon cancer.
- Two conditions — ear inflammation and benign soft-tissue tumors called adenomas — showed weak associations with the gut microbiome, suggesting that microorganisms residing in the human gut are not likely to play a role in the development of these conditions, nor are they likely to be reliable indicators that these conditions are present.
In a previous study, the HMS team used massive amounts of publicly available DNA-sequencing data from human oral and gut microbiomes to estimate the size of the universe of microbial genes in the human body. The analysis revealed that there may be more genes in the collective human microbiome than stars in the observable universe.
Given the sheer number of microbial genes that reside within the human body, the new findings represent a major step forward in understanding the complexity of the interplay between human diseases and the human microbiome, the researchers said.
“The ultimate goal of computational science is to generate hypotheses from a huge swath of data,” said Tierney. “Our work shows that this can be done and opens up so many new avenues for research and inquiry that we are only limited by the time, people, and resources needed to run those tests.”
Co-investigators included Yingxuan Tan and Aleksander Kostic.
This research was supported by the National Institutes of Health (T32 DK110919), National Science Foundation (1636870), National Institute of Allergy and Infectious Diseases (R01AI127250), American Diabetes Association Pathway to Stop Diabetes Initiator Award (1-17-INI-13), and Smith Family Awards Program for Excellence in Biomedical Research.