Despite the threat posed by breakthrough infections, CDC Director Rochelle Walensky (pictured) and Harvard infectious disease experts were unanimous that transmission still primarily occurs among the unvaccinated.
Greg Nash/Pool via AP
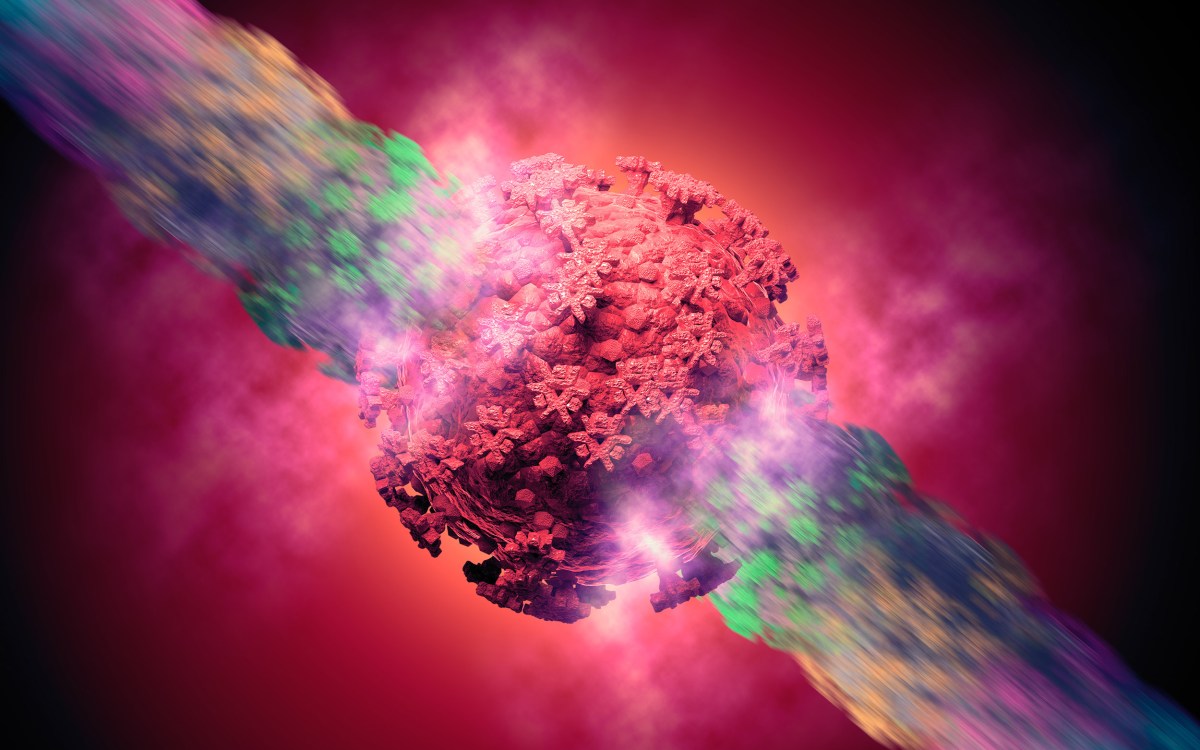
The present and future of COVID variants
Experts stress testing, vaccination amid delta surge
Last week, the Centers for Disease Control and Prevention confirmed what Harvard-affiliated physicians had reported from anecdotal and laboratory evidence: the delta variant of COVID-19 not only spreads more rapidly than other versions of the virus, it can sicken vaccinated individuals who can then spread the virus to others.
In its “Morbidity and Mortality Weekly Report,” the CDC on Friday revealed that 75 percent of patients in a cluster of 469 cases in Provincetown, Massachusetts, were vaccinated, a sobering statistic for Americans who only weeks ago were optimistic that the pandemic’s end was in sight.
“New scientific data shows that delta behaves differently than other variants,” CDC Director Rochelle Walensky said in a briefing last Wednesday. “On rare occasions, some vaccinated people may be contagious and spread the virus to others.”
Mark Poznansky, director of Massachusetts General Hospital’s Vaccine and Immunotherapy Center and an associate professor of medicine at Harvard Medical School, has seen up-close the situation Walensky discussed, including “breakthrough” cases of COVID-19 in vaccinated individuals.
Many of these patients shrug off initial symptoms, Poznansky said, attributing them to a cold or some other mild ailment. When the condition worsens, they get tested and ask for treatment advice, but the delay means that they might have been spreading the virus as they went about their lives. Poznansky, whose clinical practice at MGH is focused on immune-compromised patients who are potentially vulnerable even when vaccinated, said it’s important that vaccinated individuals get tested right away if they feel sick with COVID symptoms.
For vaccinated people who develop symptoms, “The stress should be on testing along with mask-wearing in public spaces and self-isolating where possible,” he said.
The delta variant has spread rapidly across the country, with the CDC reporting last week that it has been detected in eight in 10 samples nationally. In Massachusetts, the recent increase in cases — still at a far lower level than in U.S. hotspots — has been virtually all delta, according to Jacob Lemieux, an instructor in medicine at Harvard Medical School and an infectious disease expert at Mass General.
The World Health Organization has already designated variants Eta, Iota, Kappa, and Lamba “variants of interest” and is tracking 13 additional variants …
“We are sequencing all the cases from MGH and from the Brigham … and they’re all Delta,” said Lemieux, whose lab is conducting genetic testing on samples from COVID-19 cases. “It’s been present in the region for a couple of months, but really just over the last few weeks, just taken over.”
Paul Sax, an infectious disease expert at Brigham and Women’s Hospital, said evidence of Delta’s surge is apparent not just in lab data. The number of calls from primary care doctors seeking infectious-disease guidance has also signaled a rise in cases.
“I’d say the last three weeks or so it’s been quite noticeable, after not really seeing many cases at all,” said Sax, a professor of medicine at Harvard Medical School. “As far as hospitalizations go, our numbers are still relatively low and we’re hoping it stays that way.”
The current level of U.S. infection has already outstripped the pandemic’s initial April 2020 surge. By late last week, the seven-day average of new U.S. cases had increased nearly sevenfold from June, reaching 66,000 on July 28. Evidence from earlier in the pandemic indicates that cases are followed within a few weeks by an increase in deaths, which have risen in the seven-day average from 100 to 200 in early July to nearly 400 late in the month.
Delta exploded in India over the winter, infecting millions. In a matter of weeks, cases and deaths soared, followed by a rise in cases around the world as the new variant, believed to be roughly twice as infectious as the original, spread. Delta’s rise reinforced warnings by global experts that, in a connected world, leaving millions unvaccinated raises the likelihood that more transmissible — and even more lethal — variants will spread even to vaccinated nations.
In fact, variants have continued to develop and spread since the emergence of delta. The World Health Organization has designated variants Eta, Iota, Kappa, and Lambda “variants of interest” and is tracking 13 additional variants that originated in the U.S., Brazil, the Philippines, Indonesia, Colombia, and other nations.
Worries about delta’s ability to infect the vaccinated prompted the CDC last week to recommend that schoolchildren wear masks. (Only 30 percent of U.S. youth 12 to 17 are vaccinated.) The agency also recommended masks for vaccinated individuals living in areas of high transmission. The guidelines came after new data demonstrated that levels of virus in breakthrough infections are similar to levels in the unvaccinated. Levels of virus present in the nose and throat are important factors in COVID transmission.
Despite the threat posed by breakthrough infections, Walensky and Harvard infectious disease experts were unanimous that transmission still primarily occurs among the unvaccinated and that vaccination is the No. 1 way to fight the pandemic. In addition, though the delta variant has darkened the pandemic landscape, a bright spot is that the vaccines appear to retain their ability to protect against serious illness and death. That protection, physicians said, appears to be true even for the elderly.
What that means, physicians said, is that many of the patients who come to the hospital are younger and healthier, though unvaccinated. Patients with breakthrough infections tend to experience less severe symptoms.
“We’re seeing mostly younger people who tend to not be as ill, though we’re seeing some cases where people are quite sick,” said Robert Colgrove, interim chief of infectious diseases at Mount Auburn Hospital and an assistant professor at Harvard Medical School. “A welcome development is that totally vaccinated, frail older people with medical conditions — even among them we’re seeing very few hospitalizations, unlike in the first couple of pre-vaccine waves of the epidemic when there were just enormous amounts of very, very sick [elderly] people.”
Another potential bright spot, Sax said, is the abrupt decline in cases in the U.K., where delta cases have fallen to half of a mid-July peak of more than 60,000 daily new cases. Though the collapse in cases is poorly understood — some have speculated that the latest surge caused the nation to reach herd immunity — Sax said it is possible that Americans will see something similar.
At the end of Wednesday’s briefing, Walensky added a personal note that, after 18 months of dealing with the pandemic, the retrenchment on the agency’s masking advice was done because of its commitment to science, but was not easy.
“This new guidance weighs heavily on me. It’s not a decision taken lightly.”