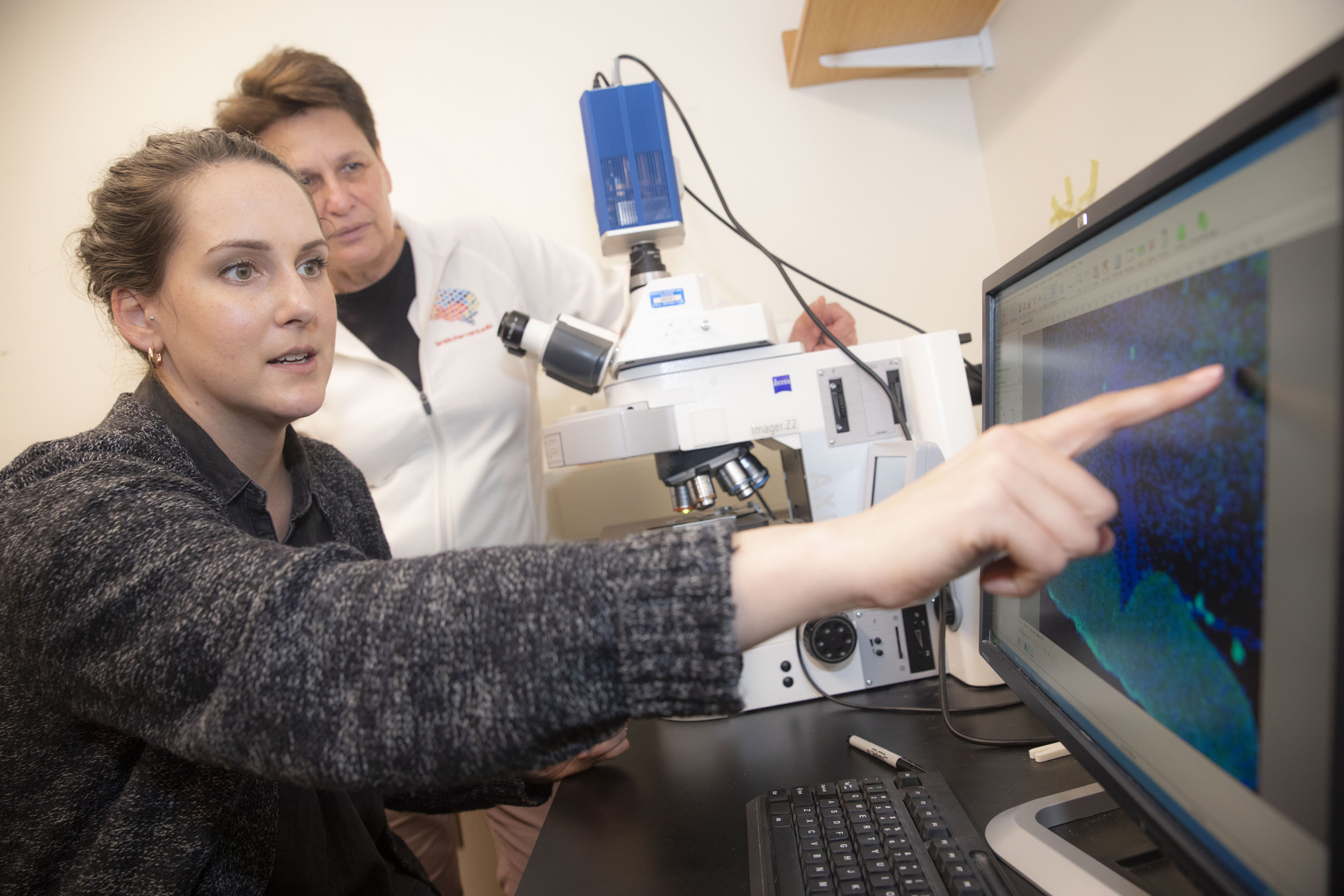
Professor Catherine Dulac (right) and postdoctoral researcher Jessica Osterhout study how the brain controls symptoms of sickness.
Kris Snibbe/Harvard Staff Photographer
How the brain responds to infection
Mouse study illuminates connections to immune system
Here’s what happens when you get an infection: The nervous system talks to the immune system to figure out that the body is under attack and then orchestrates a series of behavioral and physiological alterations that manifest as the unpleasant symptoms of sickness. For neuroscientists, longstanding questions have been: How and where does this happen in the brain?
Harvard researchers from the labs of Catherine Dulac and Xiaowei Zhuang sought the answer in the brains of mice.
In a study published in Nature, the researchers and their collaborators describe finding a small group of neurons near the base of the brain that can induce symptoms of sickness, including fever and appetite loss.
The neurons, which have not been described previously, are found in the hypothalamus, which controls key homeostatic functions that keep the body in a balanced, healthy state. The researchers discovered receptors in the neurons that are capable of detecting molecular signals coming from the immune system, an ability most neurons don’t have.
“It was important for us to establish this general principle that the brain can even sense these immune states,” said Jessica Osterhout, a postdoctoral researcher in the Dulac Lab and the study’s lead author. “This was poorly understood before.”
The researchers found that the key area of the hypothalamus is right next to the permeable blood-brain barrier, which helps circulates blood to the brain.
“What’s happening is that the cells of the blood-brain barrier that are in contact with the blood and with the peripheral immune system get activated and these non-neuronal cells secrete cytokines and chemokines that, in turn, activate the population of neurons that we found,” said Dulac, Lee and Ezpeleta Professor of Arts and Sciences and Higgins Professor of Molecular and Cellular Biology.
The hope is that scientists can one day apply the research to humans, reversing the process when it becomes a health threat.
A fever, for instance, is typically a healthy reaction that helps eliminate a pathogen. But when it gets too high, it becomes dangerous. The same can be said for loss of appetite or reduced thirst, either of which can, at first, be beneficial. But a sustained lack of nutrients or hydration can start to impede recovery.
“If we know how it works, perhaps we can help patients who have difficulty with these kinds of symptoms, like chemo patients or cancer patients, for example, who have a very low appetite but there’s really nothing we can do for them,” Osterhout said.
The work started as an effort to examine the “fever effect” in autism patients, a phenomenon in which autism symptoms fade as a patient experiences symptoms of infection. The goal was to find the neurons that generate fever and link them to the neurons that are involved with social behavior.
Instead, Osterhout found many populations of neurons that are activated when an animal is sick. She zeroed in on about 1,000 neurons in the ventral medial preoptic region of the hypothalamus because of their proximity to the blood-brain barrier.
Osterhout injected the mice with pro-inflammatory agents that mimic bacterial or viral infection. She analyzed the areas that lit up in the brain scans, and then used a powerful and precise set of methods, chemogenetics and optogenetics, to control and investigate the connectivity among the different neuronal populations. Using these tools, the researchers were able to activate or silence the neurons in command in the brains of mice and pin down their function by seeing what happened.
The researchers found that they could increase body temperature in the mice, increase warmth-seeking behavior, and decrease appetite. The neurons described in the report project to 12 brain areas, some of which are known to control thirst, pain sensation, and social interactions. This suggests that other sickness behaviors may be affected by the neuron activity in the area.
During the experiments, the scientists also noticed increased activity and activation in this population of neurons when molecules from the immune system gave off increased signals. This suggests that the brain and the immune system were communicating with each other through paracrine signaling at the ventral medial preoptic area and the blood-brain barrier right next to it. Paracrine signaling is when cells produce a signal to trigger changes in nearby cells.
Osterhout said the process expanded her understanding of how neurons work.
“As a neuroscientist, we often think of neurons activating other neurons and not that these other paracrine-type or secretion-type methods are really critical,” she said. “It changed how I thought about the problem.”
This work was supported by the National Institutes of Health and the Simons Foundation.