U.S. Marines pray over a fallen comrade after he died from wounds suffered in fighting in Fallujah, Iraq, April 8, 2004.
AP Photo/Murad Sezer, File
20 years post-invasion, many Iraq veterans haven’t found peace
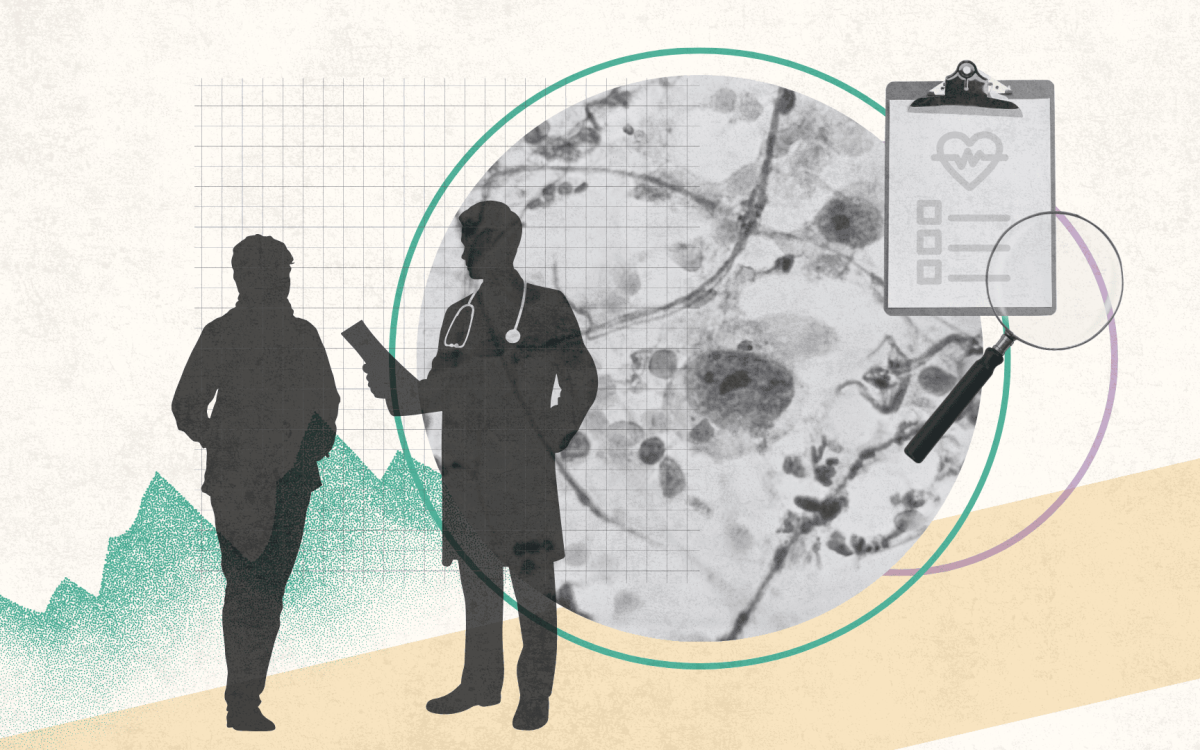
Harvard doctor who directs Home Base health program details experiences treating ‘invisible wounds,’ including efforts to keep patients from isolating
On March 20, 2003, a U.S.-led military coalition invaded Iraq, toppling the government of Saddam Hussein before a fierce insurgency rose up to oppose Western forces. As the fighting unfolded over eight years, more than a million U.S. service members deployed to the region, and many returned with complex physical and mental wounds no single treatment can erase. To mark the 20th anniversary of the invasion, the Gazette spoke with Ron Hirschberg, an assistant professor of physical medicine and rehabilitation at Harvard Medical School and a traumatic brain injury expert at Massachusetts General Hospital and Spaulding Rehabilitation Hospital. Hirschberg is also senior director of health and wellness for the veterans-focused nonprofit Home Base, where he hosts a podcast about military service and mental health. The interview has been edited for clarity and length.
Q&A
Ron Hirschberg
GAZETTE: Is there still a lot of pain among veterans who served in Iraq and are dealing with traumatic brain injury, post-traumatic stress, depression, and other conditions?
HIRSCHBERG: When the war stops and the coverage of Iraq and Afghanistan stops, the people who served there — whether it’s one deployment or 10, whether they were there 20 years ago or two years ago before Kabul fell — those wounds are not like bones that break and heal in 12 weeks. They can resurface months to years later, and then it’s a matter of dampening the symptoms and providing the right care so that they can live their lives. In fact, we can expect even more need as time passes — as service members try to re-engage with civilian life and those who have difficulty doing it become isolated. Part of what triggers post-traumatic stress and exacerbates these wounds is not feeling connected to a group anymore.
GAZETTE: We’re marking the anniversary of the start of the Iraq War. Is it possible and/or necessary to separate Iraq service from Afghanistan service when talking about these injuries?
HIRSCHBERG: More than 1.8 million Iraq and Afghanistan veterans returned home with a permanent disability, with close to 1 million of these linked to mental health and traumatic brain injuries, not to mention the moral injuries and complicated survivor guilt that present their own unique and complex challenges. When it comes to Afghanistan, there’s a feeling you left with loose ends, and feelings of guilt with no ability to help. Many of our veterans developed strong bonds with families and translators, and many of these people continued to face grave threats after our withdrawal from Kabul.
“Part of what triggers post-traumatic stress and exacerbates these wounds is not feeling connected to a group anymore.”
GAZETTE: You mentioned that these conditions can endure forever. What is the proportion of those who recover?
HIRSCHBERG: Recovery is a process. My job at MGH is to see people with moderate to severe traumatic brain injury. When you see someone come in after a car accident, during day two to day four, they’re getting stabilized. The next week, they start to heal. They will recover for not just days to weeks, but really months to years. In six months to one year, you’re going to see a lot of that recovery. People can heal such that they can live their lives, have good family relationships. They might get back to work, travel, and live functional lives. I would use an analogy of chronic medical conditions like diabetes or cancer in remission. You are not going to fix them, but you can manage people with more diagnostic understanding and treatment.
When we look at Vietnam, at the veterans who are now 50 years post-deployment, we see folks who have had post-traumatic stress and other symptoms rear their head decades out. A classic situation is retirement or going on to the next chapter in life. Then there’s a loss of purpose and maybe isolation that bring on those symptoms. Even watching what’s going on in Ukraine can be a trigger.
GAZETTE: So there are people who may not have suffered initially and are now experiencing symptoms many years later?
HIRSCHBERG: It’s possible that some were treated and did well for many years and then one day they find themselves in trouble. We know that, among all veterans, there are 20 suicides a day, and between 2015 and 2020 there was about a 40 percent increase in suicides among active-duty service members. Thirty thousand veterans have died by suicide in just the Operation Iraqi Freedom and Operation Enduring Freedom conflicts over 20 years. Since 9/11, there have been more than 125,000 deaths by suicide of all-era veterans.
GAZETTE: When we talk about these invisible wounds of war, are they dependent on the specific type of injury or do they depend heavily on factors related to the individual?
HIRSCHBERG: Who you are — your medical history, social factors, psychiatric factors — matters. Then there’s the injury itself and post-injury. Rehab and recovery are very much affected by society and can be affected by belonging or lack of belonging. It’s like a tribe, really, of folks who have not only a sense of belonging but also a real sense of purpose. Part of the management of these invisible wounds is about finding new connections and new purpose.
“Among all veterans, there are 20 suicides a day, and between 2015 and 2020 there was about a 40 percent increase in suicides among active-duty service members.”
GAZETTE: Has there been progress in the science of understanding and treating these conditions?
HIRSCHBERG: Home Base has a standard of care at its core, like insulin for diabetes or chemotherapy for cancer. The standard includes prolonged exposure therapy, cognitive processing therapy, and cognitive behavioral therapy. For traumatic brain injury, it’s cognitive rehab therapy and vestibular/physical therapy. Data indicates that these therapies work. But colleagues at Spaulding, Mass General Brigham, and Home Base are looking to improve them, trying to find biomarkers of post-traumatic stress and traumatic brain injury and how they may impact treatment. We’re doing work in psychedelics and have a partnership with MGH’s Center for the Neuroscience of Psychedelics and we’ve done some work in virtual reality for PTS. We are proud of our wellness efforts, getting people together in the kitchen with dietitians and in the gym with strength and conditioning coaches. We also incorporate art therapy and music, which tap into more creative spaces and have been shown to help with stress and depression.
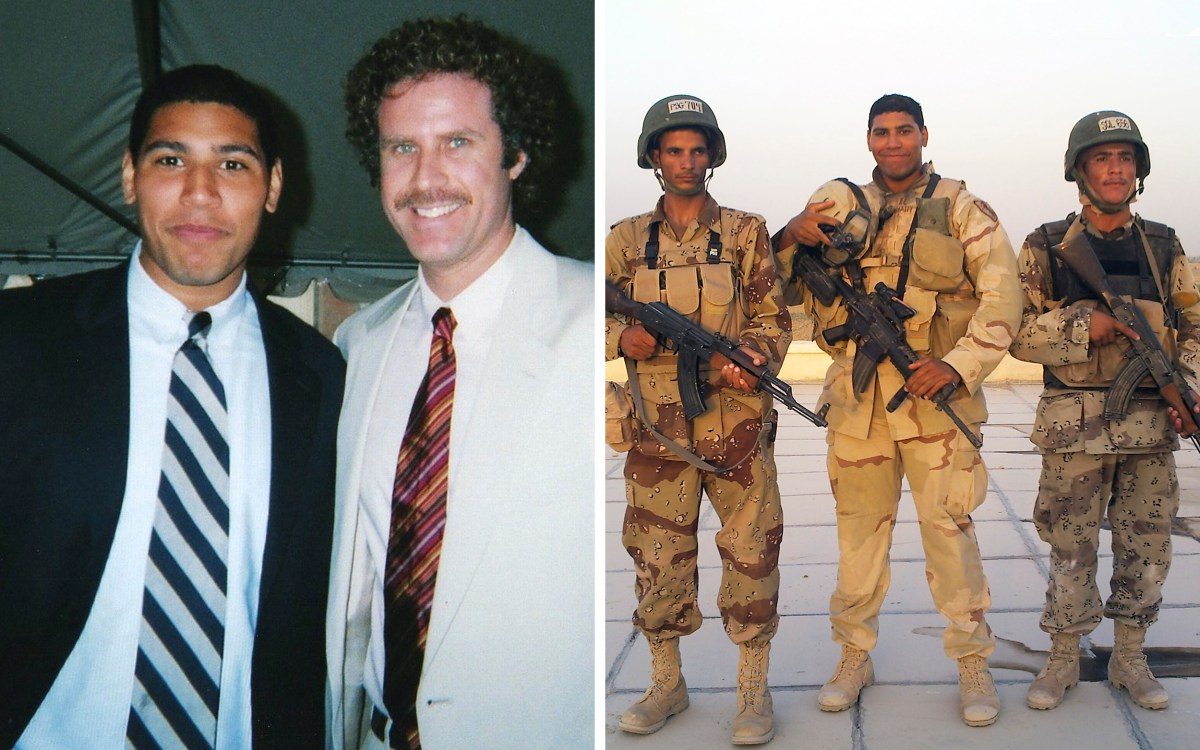
GAZETTE: Why do you do this work?
HIRSCHBERG: I have not served in the military and every day that I’m there, I’m reminded that our job is to take care of the folks who have raised their hand to take care of us. Julian Kitching, a Green Beret, and his brother, an Army Ranger, came through our program. Julian said at the Run to Home Base last year that service members sign up to go to combat to keep us safe. The last thing anyone wants is to go to war, but when you have to, that’s what they’re there to do. The other end of the equation is simple: We take care of them when they’re back.