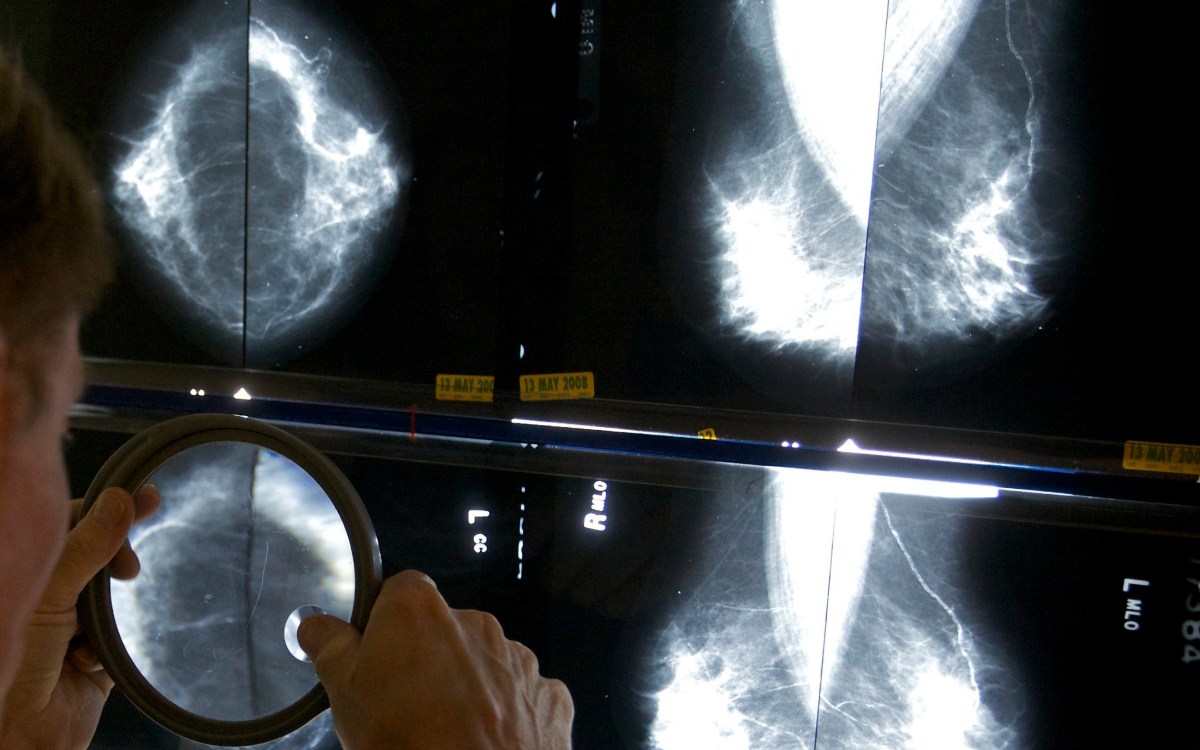
AP file photo
When to get first mammogram? Doctor explains latest advice.
Reversal puts guidance ‘back in line’ with experts who ‘never stopped recommending’ breast cancer screening start at age 40
Women should start getting regular mammograms at the age of 40, according to a new recommendation being drafted by the U.S. Preventive Services Task Force. This is a reversal from the previous recommendation of age 50, which means more than 20 million women will now be considering mammogram screening. In order to better understand the implications of this change, the Gazette spoke with Steven Isakoff, the director of Breast Cancer Clinical Research at Mass General Cancer Center and an assistant professor at Harvard Medical School. The following interview has been edited for length and clarity.
Q&A
Steven Isakoff
GAZETTE: In the past, mammogram screening started at age 40. But in 2009, it was increased to age 50. And now it’s reversing back to age 40. Why?
ISAKOFF: In the U.S. breast cancer treatment community, we’ve generally felt that it never should have changed from 40. So for us, this is back in line with what we’ve generally recommended. The reason that it changed from 40 to 50 was a decision from the task force that the benefits did not outweigh the perceived harms. And the harms that were considered in their evaluation were things like the psychological impact and anxiety associated with getting a false positive, the risk of a biopsy, or the risk of additional follow-up. And there was a concern when these guidelines came out many years ago that it was a bit paternalistic to say, “Well, we think causing anxiety for women is a harm, so we’re going to change the age to 50 when the likelihood of finding cancer is a little higher.”
Most patients will tell you that if there’s a chance of finding their cancer a little earlier — with a small chance of a false positive — that’s OK. The other thing to consider is most of the false positives are picked up on a screening mammogram. What that means is the patient gets called back for a diagnostic mammogram. Generally, these do not lead to surgical interventions that are unnecessary. In the majority of cases, it’s simply a call back for more imaging, which most of the time results in “nothing to see here” and the patient goes back to regular screening.

GAZETTE: Since we’re seeing an uptick in young women getting breast cancer, is this a situation where the benefits are outweighing those risks?
ISAKOFF: From the committee’s description in the guidelines, that seems to be what changed. They reported that between 2015 and 2019, the annual incidence of breast cancer in the younger population increased by about 2 percent each year. And that crossed a threshold where they felt that screening at that age makes sense. As the incidence of the disease in the population changes, then the benefit of screening can change as well. And that seems to be what they’re referring to with this most recent change.
GAZETTE: Black women, who die of breast cancer at twice the rate of white women of the same age, may benefit from earlier screening. Do you think earlier screening could affect that racial disparity we’re seeing?
ISAKOFF: We sure hope so. Black women report screening at the same rates as white women. And that implies that access to screening itself, or the desire to do screening, isn’t the reason for the disparity. But with an increasing rate or incidence of breast cancer in younger Black women, making this screening technology available to them will help. But there are a couple of important points. One is younger women in general, compared to older women, tend to get more aggressive types of breast cancer. And Black women compared to non-Black women tend to get more aggressive types of breast cancer. And it’s well-recognized that those kinds of cancers may not be optimally identified by screening because they tend to grow a little bit faster. They can often be the cancers that are picked up in the interval between screenings. We have to recognize that we need more than just screening.
The other point I would make is that it’s equally important — if not more important — to make sure that after screening, cancer patients are provided equitable care for the follow-up diagnostic studies and treatment. I think that’s going to make a really big impact, more than just screening.
“Between 2015 and 2019, the annual incidence of breast cancer in the younger population increased by about 2 percent each year.”
GAZETTE: This new recommendation is going to affect more than millions of women. How do you think that will impact the healthcare system?
ISAKOFF: In Massachusetts, for the most part, we’ve never stopped recommending 40. I think we’re fortunate to be in a state that is very supportive of equitable healthcare and committed to improving it. But I have heard from colleagues around the country where they had actually changed the age to 50. So will there be some cost to the healthcare system there? Probably, but mammograms are a fairly cheap test to do. And we hope in the long run, it will actually help because it’ll diagnose cancers earlier when they’re more treatable and require less aggressive treatment. Hopefully it will have a positive impact on the healthcare system because it’ll have less people with advanced disease, which is when the cost of care gets very expensive.
GAZETTE: How do you see this new recommendation benefiting both patients and providers?
ISAKOFF: I think the benefit is it provides a little bit more consistency. Often, medicine is not a black-and-white decision. It can be very troubling for patients when they see differing opinions. There are still some discrepancies in breast cancer screening, but at least the recommendation states that it is now generally recommended to start earlier. From the provider side, it will help ensure that these screenings are paid for; we certainly have heard of cases around the country where some organizations or insurers were no longer covering mammograms from ages 40 to 50. So this will help restore that. And I think it allows us, as providers, to really support the value of mammographic screening and potentially reduce long-term mortality from breast cancer.