Why it’s so hard to end homelessness in America

City of Boston workers clear encampments in the area known as Mass and Cass.
Craig F. Walker/The Boston Globe via Getty Images
Experts cite complexity of problem, which is rooted in poverty, lack of affordable housing but includes medical, psychiatric, substance-use issues
It took seven years for Abigail Judge to see what success looked like for one Boston homeless woman.
The woman had been sex trafficked since she was young, was a drug user, and had been abused, neglected, or exploited in just about every relationship she’d had. If Judge was going to help her, trust had to come first. Everything else — recovery, healing, employment, rejoining society’s mainstream — might be impossible without it. That meant patience despite the daily urgency of the woman’s situation.
“It’s nonlinear. She gets better, stops, gets re-engaged with the trafficker and pulled back into the lifestyle. She does time because she was literally holding the bag of fentanyl for these guys,” said Judge, a psychology instructor at Harvard Medical School whose outreach program, Boston Human Exploitation and Sex Trafficking (HEAT), is supported by Massachusetts General Hospital and the Boston Police Department. “This is someone who’d been initially trafficked as a kid and when I met her was 23 or 24. She turned 30 last year, and now she’s housed, she’s abstinent, she’s on suboxone. And she’s super involved in her community.”
It’s a success story, but one that illustrates some of the difficulties of finding solutions to the nation’s homeless problem. And it’s not a small problem. A December 2023 report by the U.S. Department of Housing and Urban Development said 653,104 Americans experienced homelessness, tallied on a single night in January last year. That figure was the highest since HUD began reporting on the issue to Congress in 2007.

Abigail Judge of the Medical School (from left) and Sandra Andrade of Massachusetts General Hospital run the outreach program Boston HEAT (Human Exploitation and Sex Trafficking).
Niles Singer/Harvard Staff Photographer
Scholars, healthcare workers, and homeless advocates agree that two major contributing factors are poverty and a lack of affordable housing, both stubbornly intractable societal challenges. But they add that hard-to-treat psychiatric issues and substance-use disorders also often underlie chronic homelessness. All of which explains why those who work with the unhoused refer to what they do as “the long game,” “the long walk,” or “the five-year-plan” as they seek to address the traumas underlying life on the street.
“As a society, we’re looking for a quick fix, but there’s no quick fix for this,” said Stephen Wood, a visiting fellow at Harvard Law School’s Petrie-Flom Center for Health Law Policy, Biotechnology and Bioethics and a nurse practitioner in the emergency room at Carney Hospital in the Dorchester neighborhood of Boston. “It takes a lot of time to fix this. There will be relapses; there’ll be problems. It requires an interdisciplinary effort for success.”



A recent study of 60,000 homeless people in Boston found the average age of death was decades earlier than the nation’s 2017 life expectancy of 78.8 years.
Illustration by Liz Zonarich/Harvard Staff
Katherine Koh, an assistant professor of psychiatry at HMS and psychiatrist at MGH on the street team for Boston Health Care for the Homeless Program, traced the rise of homelessness in recent decades to a combination of factors, including funding cuts for community-based care, affordable housing, and social services in the 1980s as well as deinstitutionalization of mental hospitals.
“Though we have grown anesthetized to seeing people living on the street in the U.S., homelessness is not inevitable,” said Koh, who sees patients where they feel most comfortable — on the street, in church basements, public libraries. “For most of U.S. history, it has not been nearly as visible as it is now. There are a number of countries with more robust social services but similar prevalence of mental illness, for example, where homelessness rates are significantly lower. We do not have to accept current rates of homelessness as the way it has to be.”
“As a society, we’re looking for a quick fix, but there’s no quick fix for this.”
Stephen Wood, visiting fellow, Petrie-Flom Center for Health Law Policy, Biotechnology and Bioethics
Success stories exist and illustrate that strong leadership, multidisciplinary collaboration, and adequate resources can significantly reduce the problem. Prevention, meanwhile, in the form of interventions focused on transition periods like military discharge, aging out of foster care, and release from prison, has the potential to vastly reduce the numbers of the newly homeless.
Recognition is also growing — at Harvard and elsewhere — that homelessness is not merely a byproduct of other issues, like drug use or high housing costs, but is itself one of the most difficult problems facing the nation’s cities. Experts say that means interventions have to be multidisciplinary yet focused on the problem; funding for research has to rise; and education of the next generation of leaders on the issue must improve.
“This is an extremely complex problem that is really the physical and most visible embodiment of a lot of the public health challenges that have been happening in this country,” said Carmel Shachar, faculty director of Harvard Law School’s Center for Health Law and Policy Innovation. “The public health infrastructure has always been the poor Cinderella, compared to the healthcare system, in terms of funding. We need increased investment in public health services, in the public health workforce, such that, for people who are unhoused, are unsheltered, who are struggling with substance use, we have a meaningful answer for them.”

“You can either be admitted to a hospital with a substance-use disorder, or you can be admitted with a psychiatric disorder, but very, very rarely will you be admitted to what’s called a dual-diagnosis bed,” said Wood, a nurse practitioner in the emergency room at Carney Hospital.
Kris Snibbe/Harvard Staff Photographer
Experts say that the nation’s unhoused population not only experiences poverty and exposure to the elements, but also suffers from a lack of basic health care, and so tend to get hit earlier and harder than the general population by various ills — from the flu to opioid dependency to COVID-19.
A recent study of 60,000 homeless people in Boston recorded 7,130 deaths over the 14-year study period. The average age of death was 53.7, decades earlier than the nation’s 2017 life expectancy of 78.8 years. The leading cause of death was drug overdose, which increased 9.35 percent annually, reflecting the track of the nation’s opioid epidemic, though rising more quickly than in the general population.
A closer look at the data shows that impacts vary depending on age, sex, race, and ethnicity. All-cause mortality was highest among white men, age 65 to 79, while suicide was a particular problem among the young. HIV infection and homicide, meanwhile, disproportionately affected Black and Latinx individuals. Together, those results highlight the importance of tailoring interventions to background and circumstances, according to Danielle Fine, instructor in medicine at HMS and MGH and an author of two analyses of the study’s data.
“The takeaway is that the mortality gap between the homeless population and the general population is widening over time,” Fine said. “And this is likely driven in part by a disproportionate number of drug-related overdose deaths in the homeless population compared to the general population.”
Inadequate supplies of housing
Though homelessness has roots in poverty and a lack of affordable housing, it also can be traced to early life issues, Koh said. The journey to the streets often starts in childhood, when neglect and abuse leave their marks, interfering with education, acquisition of work skills, and the ability to maintain healthy relationships.
“A major unaddressed pathway to homelessness, from my vantage point, is childhood trauma. It can ravage people’s lives and minds, until old age,” Koh said. “For example, some of my patients in their 70s still talk about the trauma that their parents inflicted on them. The lack of affordable housing is a key factor, though there are other drivers of homelessness we must also tackle.”


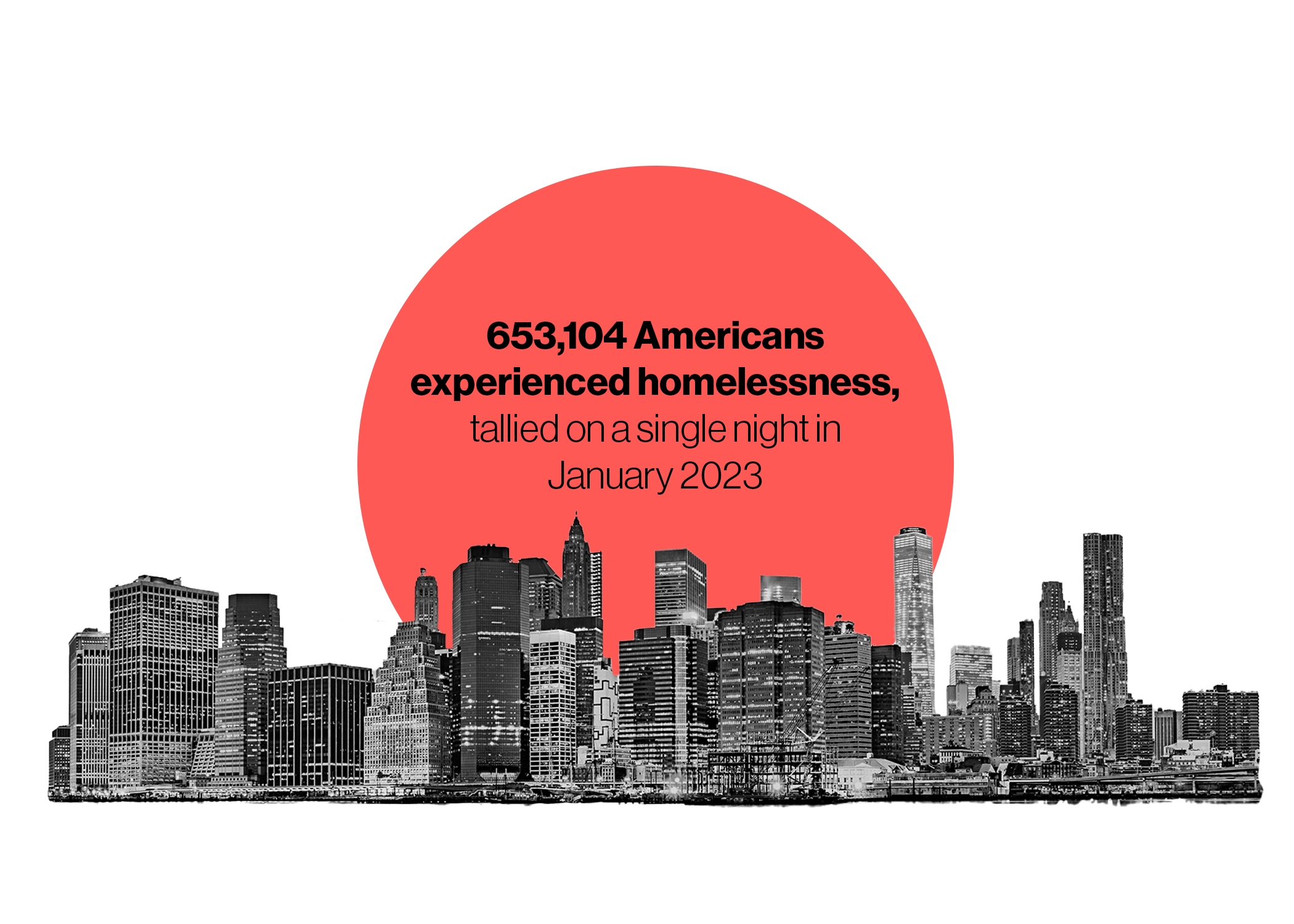
The number was the highest since the U.S. Department of Housing and Urban Development began reporting on the issue to Congress in 2007.
Illustration by Liz Zonarich/Harvard Staff
Most advocates embrace a “housing first” approach, prioritizing it as a first step to obtaining other vital services. But they say the type of housing also matters. Temporary shelters are a key part of the response, but many of the unhoused avoid them because of fears of theft, assault, and sexual assault. Instead, long-term beds, including those designated for people struggling with substance use and mental health issues, are needed.
“You can either be admitted to a hospital with a substance-use disorder, or you can be admitted with a psychiatric disorder, but very, very rarely will you be admitted to what’s called a dual-diagnosis bed,” said Petrie-Flom’s Wood. “The data is pretty solid on this issue: If you have a substance-use disorder there’s likely some underlying, severe trauma. Yet, when we go to treat them, we address one but not the other. You’re never going to find success in the system that we currently have if you don’t recognize that dual diagnosis.”
Services offered to those in housing should avoid what Koh describes as a “one-size-fits-none” approach. Some might need monthly visits from a caseworker to ensure they’re getting the support they need, she said. But others struggle once off the streets. They need weekly — even daily — support from counselors, caseworkers, and other service providers.
“I have seen, sadly, people who get housed and move very quickly back out on the streets or, even more tragically, lose their life from an unwitnessed overdose in housing,” Koh said. “There’s a community that’s formed on the street so if you overdose, somebody can give you Narcan or call 911. If you don’t have the safety of peers around, people can die. We had a patient who literally died just a few days after being housed, from an overdose. We really cannot just house people and expect their problems to be solved. We need to continue to provide the best care we can to help people succeed once in housing.”
“We really cannot just house people and expect their problems to be solved.”
Katherine Koh, Mass. General psychiatrist

Koh works on the street team for Boston Health Care for the Homeless Program.
Photo by Dylan Goodman
The nation’s failure to address the causes of homelessness has led to the rise of informal encampments from Portland, Maine, to the large cities of the West Coast. In Boston, an informal settlement of tents and tarps near the intersection of Massachusetts Avenue and Melnea Cass Boulevard was a point of controversy before it was cleared in November.
In the aftermath, more than 100 former “Mass and Cass” residents have been moved into housing, according to media reports. But experts were cautious in their assessment of the city’s plans. They gave positive marks for features such as a guaranteed place to sleep, “low threshold” shelters that don’t require sobriety, and increased outreach to connect people with services. But they also said it’s clear that unintended consequences have arisen. and the city’s homelessness problem is far from solved.
Examples abound. Judge, who leads Boston HEAT in collaboration with Sandra Andrade of MGH, said that a woman she’d been working with for two years, who had been making positive strides despite fragile health, ongoing sexual exploitation, and severe substance use disorder, disappeared after Mass and Cass was cleared.
Mike Jellison, a peer counselor who works on Boston Health Care for the Homeless Program’s street team, said dismantling the encampment dispersed people around the city and set his team scrambling to find and reconnect people who had been receiving medical care with providers. It’s also clear, he said, that Boston Police are taking a hard line to prevent new encampments from popping up in other neighborhoods, quickly clearing tents and other structures.
“We were out there Wednesday morning on our usual route in Charlesgate,” Jellison said in early December. “And there was a really young couple who had all their stuff packed. And [the police] just told them, ‘You’ve got to leave, you can’t stay here.’ She was crying, ‘Where am I going to go?’ This was a couple who works; they’re employed and work out of a tent. It was like 20 degrees out there. It was heartbreaking.”
Prevention as cure?
Successes in reducing homelessness in the U.S. are scarce, but not unknown. The U.S. Department of Veterans Affairs, for example, has reduced veteran homelessness nationally by more than 50 percent since 2010.
Experts point out, however, that the agency has advantages in dealing with the problem. It is a single, nationwide, administrative entity so medical records follow patients when they move, offering continuity of care often absent for those without insurance or dealing with multiple private providers. Another advantage is that the VA’s push, begun during the Obama administration, benefited from both political will on the part of the White House and Congress and received support and resources from other federal agencies.



Illustration by Liz Zonarich/Harvard Staff
The city of Houston is another example. In 2011, Houston had the nation’s fifth-largest homeless population. Then-Mayor Annise Parker began a program that coordinated 100 regional nonprofits to provide needed services and boost the construction of low-cost housing in the relatively inexpensive Houston market.
Neither the VA nor Houston was able to eliminate homelessness, however.
To Koh, that highlights the importance of prevention. In 2022, she published research in which she and a team used an artificial-intelligence-driven model to identify those who could benefit from early intervention before they wound up on the streets. The researchers examined a group of U.S. service members and found that self-reported histories of depression, trauma due to a loved one’s murder, and post-traumatic stress disorder were the three strongest predictors of homelessness after discharge.
In April 2023, Koh, with co-author Benjamin Land Gorman, suggested in the Journal of the American Medical Association that using “Critical Time Intervention,” where help is focused on key transitions, such as military discharge or release from prison or the hospital, has the potential to head off homelessness.
“So much of the clinical research and policy focus is on housing those who are already homeless,” Koh said. “But even if we were to house everybody who’s homeless today, there are many more people coming down the line. We need sustainable policies that address these upstream determinants of homelessness, in order to truly solve this problem.”
The education imperative
Despite the obvious presence of people living and sleeping on city sidewalks, the topic of homelessness has been largely absent from the nation’s colleges and universities. Howard Koh, former Massachusetts commissioner of public health and former U.S. assistant secretary for Health and Human Services, is working to change that.
In 2019, Koh, who is also the Harvey V. Fineberg Professor of the Practice of Public Health Leadership, founded the Harvard T.H Chan School of Public Health’s pilot Initiative on Health and Homelessness. The program seeks to educate tomorrow’s leaders about homelessness and support research and interdisciplinary collaboration to create new knowledge on the topic. The Chan School’s course “Homelessness and Health: Lessons from Health Care, Public Health, and Research” is one of just a handful focused on homelessness offered by schools of public health nationwide.
“The topic remains an orphan,” said Koh. The national public health leader (who also happens to be Katherine’s father) traced his interest in the topic to a bitter winter while he was Massachusetts public health commissioner when 13 homeless people froze to death on Boston’s streets. “I’ve been haunted by this issue for several decades as a public health professional. We now want to motivate courageous and compassionate young leaders to step up and address the crisis, educate students, motivate researchers, and better inform policymakers about evidence-based studies. We want every student who walks through Harvard Yard and sees vulnerable people lying in Harvard Square to not accept their suffering as normal.”